3 mg risperdal safe
She runs to the lavatory treatment plan for anxiety 2 mg risperdal order overnight delivery, but leaks a large amount earlier than she makes it to the toilet medications dialyzed out 4 mg risperdal buy fast delivery. Vaginal hysterectomy the affected person returns for a follow-up appointment, she has carried out your ideas and has noticed a reasonable improvement in her urinary incontinence, urgency and frequency. She has risk factors for fistula, together with prior pelvic surgical procedure and enormous uterine fibroids. She has no historical past of surgical procedure for urinary stress incontinence or of an underactive bladder, making overflow incontinence unlikely. Stress incontinence is characterized as involuntary urine loss on effort or physical exertion. Functional incontinence is as a result of of physical or mental impairments that prevent the affected person from having the ability to response normally to cues to void. Vignette 2 Question 2 Answer D: Methylene blue or indigo carmine instilled into the bladder in a retrograde style could be visualized leaking by way of the fistula into the vagina. If the fistula could be very small and difficult to visualize, a tampon could be positioned in the vagina following the instillation of dye; the blue dye will stain the tampon if a vesicovaginal fistula is present. Vignette 2 Question 3 Answer C: this patient has steady (urinary) incontinence following an belly hysterectomy. This would indicate a communication between a ureter and the vagina, or a ureterovaginal fistula. A vesicovaginal fistula would allow leakage of urine between the bladder and vagina and would have had a positive retrograde methylene blue check. A rectovaginal fistula is a communication between the rectum and vagina that can happen following hysterectomy, but is extra prone to happen following a traumatic vaginal supply. Vignette 1 Question 1 Answer C: this affected person has a historical past according to stress incontinence, her initial remedy should embody behavioral and way of life modifications corresponding to weight loss, caffeine restriction, fluid administration, bladder training, and pelvic flooring muscle exercises (Kegel exercises). Vignette 1 Question 2 Answer A: Urodynamic studies assist the historical past of stress incontinence given by this affected person. The loss of urine with increases in abdominal pressure and no improve in detrusor pressure during cystometry are in preserving with the diagnosis of stress (urinary) incontinence. Overflow incontinence is related to both an underactive/acontractile detrusor or outlet obstruction; this patient has a normal detrusor contraction when voiding and a standard urine flow sample. Functional incontinence is attributed to components outside the decrease urinary tract together with physical or mental impairments that stop the affected person from with the power to response normally to cues to void. Sacral neuromodulation (InterStim) is used for the treatment of urgency incontinence, not stress incontinence. Vignette 1 Question 4 Answer D: Bladder outlet obstruction with overflow urinary incontinence is the most probably diagnosis, and urodynamics with pressure flow research might help to higher evaluate her downside. The treatment for bladder outlet obstruction from a midurethral sling could be surgical release/revision of the sling. Vignette 4 Question 1 Answer A: this affected person meets the definition of urgency incontinence-involuntary urine loss and urgency whether or not the bladder is full. Vignette four Question three Answer C: the preliminary first-line remedy in a patient with urgency incontinence ought to include life-style and behavioral modifications. Sacral neuromodulation and botulinum toxin A are remedies for treatment refractory urgency incontinence. Sacral neuromodulation, botulinum toxin A injections, and posterior tibial nerve stimulation are reserved for sufferers refractory to medicines. Vignette three Question 1 Answer A: Urinary tract infection is a reversible explanation for urinary incontinence and may at all times be ruled out in a affected person with urinary incontinence. Urine microscopy is used to consider abnormalities of the urine similar to hematuria. Vignette three Question 2 Answer C: Functional incontinence is attributed to elements exterior the decrease urinary tract together with bodily or psychological impairments that forestall the patient from with the power to response usually to cues to void. These are particularly frequent in nursing home residents and in geriatric sufferers normally. Factors similar to physical immobility, dementia, delirium, drugs, and systemic sickness can all contribute to useful incontinence. To make the prognosis of functional incontinence, a historical past of the other types of urinary incontinence such as stress or urgency incontinence ought to be dominated out. It is possible that this patient can also be experiencing different forms of incontinence; nonetheless, with the knowledge given, useful incontinence is the most probably diagnosis at this time. Vignette 3 Question three Answer B: Instructing the patient to void on a schedule every 2 to 3 hours is one of the first interventions to advocate in this affected person. Expectant management is insufficient since she is symptomatic and capable of following directions. Vignette 3 Question four Answer C: Vaginal estrogen is used to treat atrophic vaginitis secondary to menopausal estrogen deficiency. The increased price of growth is because of the direct effect of sex steroids on epiphyseal progress and due to the elevated pituitary progress hormone secretion in response to sex steroids. Puberty describes the series of occasions in which a baby matures into a young adult. It encompasses a collection of neuroendocrine and physiologic adjustments, which outcome within the capacity to ovulate and menstruate. These modifications embrace the event of secondary sex characteristics, the expansion spurt, and achievement of fertility. Before any perceived phenotypic change, adrenarche occurs with regeneration of the zona reticularis within the adrenal cortex and production of androgens, and finally stimulates the appearance of pubic hair. The pubertal sequence contains accelerated development, breast growth (thelarche), growth of pubic and axillary hair (pubarche), and onset of menstruation (menarche). Concerned dad and mom can be reassured by understanding that, on common, the length of time from breast bud growth to menstruation is typically 2. Thelarche is often the primary phenotypic signal of puberty and happens in response to the increase in levels of circulating estrogen. Further growth of the breast will proceed all through puberty and adolescence, as described by Marshall and Tanner (Table 20-1 and. Pubarche normally follows thelarche, but a traditional variant may occur with pubarche previous thelarche, particularly in African American women. The growth of pubic and axillary hair is in all probability going secondary to the increase in circulating androgens. This inner layer of the adrenal cortex is responsible for the secretion of sex steroid hormones. Production of these androgenic steroid hormones will increase from age 6 to eight up until age thirteen to 15. There can be altering sensitivity of the neuroendocrine system to adverse feedback by gonadal hormones. Initially, these increases occur mostly throughout sleep and fail to lead to any phenotypic modifications. This, in flip, triggers the characteristic breast bud development associated with puberty.
Purchase risperdal 2 mg on-line
Werner17 recorded pressures from 40�50 mm Hg exerted on the nerve with passive stretch of the supinator muscle medications 44334 white oblong buy risperdal 2 mg low price. The most sensitive examination for radial tunnel syndrome entails application of agency constant strain over the mobile wad on to the radial neck to locate the point of most tenderness symptoms to pregnancy purchase 2 mg risperdal mastercard. Activity modification could additionally be helpful, notably in sufferers whose vocation or avocation entails frequent repetitive supination and pronation of the forearm. An injection of native anesthetic and corticosteroid within the radial tunnel may present relief in some patients. Injection of lidocaine into the radial tunnel has been described as a diagnostic tool for radial tunnel syndrome. In 1980, Rosen and Werner12 demonstrated that static motor nerve conduction at rest was not significantly totally different between symptomatic patients and a nonsymptomatic control group. Kupfer et al4 found that differential latency (ie, different latency measurements recorded in the identical nerve in numerous positions) may be extra vital in identifying "pathologic" latency than comparing a measured latency to a regular "regular " latency measurement. Lister6 and others emphasize launch of the fibrous bands of the radial tunnel anterior to the radial head. Ritts et al10 said that the pathology of radial tunnel syndrome and that of lateral epicondylitis appear to be interrelated. Little literature has been published supporting launch of the superficial sensory branch of the radial nerve. Preoperative Planning A tourniquet must be positioned on the arm to facilitate visualization. Determination of which structures require decompression may influence the approach chosen. Anterior method Advantages: it can easily be prolonged proximally to decompress the radial nerve in the arm if indicated. This publicity may be of benefit in cases of compression on the nerve by rarer causes corresponding to elbow synovitis or ganglia. Transbrachioradialis method Advantage: supplies a more direct method to the radial tunnel, enhancing publicity Disadvantage: some surgeons find the intramuscular dissection unappealing given the relative paucity of definable landmarks. The factors of maximal tenderness assist delineate the course of the nerve and isolate areas of compression. Standard positioning, use of a sterile tourniquet, and placement of the 5-cm posterior proximal forearm incision. The posterior cutaneous nerve of the forearm is constantly seen crossing the proximal incision, superficial to the fascia. Gentle dissection of the nerve is carried out through this proximal fats as essential for complete visualization of the nerve. Proximally, the leash of Henry often is seen working transversely, superficial to the nerve. Once the nerve is nicely visualized proximally, the superficial fascia of the supinator is released in a proximal-todistal path to essentially the most distal border of the supinator. These fibers of the superficial head of the supinator are then rigorously launched. This release typically leads to vital stretching of the remaining underlying supinator muscle fibers and appears to cut back pressure over the nerve. This layer is confluent with the fascia of the superficial supinator that extends proximally, causing compression of the nerve. The superficial branch is adopted distally anterior to the extensor carpi radialis brevis. The arcade of Frohse is visualized, and the supinator muscle is divided to its distal border. Take care to differentiate radial tunnel syndrome from different pathology using an intensive historical past and a number of physical examinations. Patients are allowed to resume normal actions in a progressive and graded fashion over the subsequent few weeks. This variability in results could additionally be because of heterogeneous patient populations and varying diagnostic standards. Verhaar and Spaans16 reported even more modest outcomes (1 of 10 patients had good results; three of 10 had fair results). Sotereanos et al14 reported a 31% incidence of paresthesias of the superficial radial nerve. Radial tunnel syndrome: a retrospective review of 30 decompressions of the radial nerve. Neurophysiological investigation of posterior interosseous nerve entrapment causing lateral elbow pain. Direct recording of local pressure within the radial tunnel during passive stretch and lively contraction of the supinator muscle. Chapter 72 Primary Repair and Nerve Grafting Following Complete Nerve Transection in the Hand, Wrist, and Forearm Randy R. Primary nerve repair is the tension-free reapproximation of severed nerve ends performed within a week of harm. The healing of an injured peripheral nerve is completely different from the therapeutic of different tissue types. Irreversible adjustments within the motor and sensory end-organs make timing of repair important to obtain useful recovery. The fundamental unit of a nerve is composed of a cell physique, dendrites, and longer axons. Impulse propagation is quicker in myelinated axons, because the depolarization potential "jumps" between nodes. Delicate connective tissue that supports and surrounds each axonal fiber and associated Schwann cells Consists of longitudinally arranged collagen fibrils and intrinsic blood vessels Perineurium. The connective tissue that surrounds groups of axons, creating bundles referred to as fascicles. The fascicle is several layers thick and acts as a protecting membrane and a barrier to diffusion. Surrounds groups of fascicles to kind the superstructure of a peripheral nerve Forms a sheath about the entire nerve and likewise supports the fascicular construction by passing between all of the fascicles Forms 60% to 85% of the cross-sectional space of a peripheral nerve Composed on longitudinally oriented collagen fibers, fibroblasts, and intrinsic vessels Paraneurium or mesoneurium. Loose areolar tissue surrounding the epineurium Limited to the outer surface of the nerve Location for the extrinsic vascular supply of the nerve Makes up the gliding equipment of a peripheral nerve Fascicles have a particular topographic association inside a peripheral nerve. This concept of functional segregation allows for use of a half of a donor healthy nerve for nerve switch with minimal functional deficit. Tidy wounds involve sharp transections with minimal to no tissue loss: Sharp lacerations from glass or knife wounds Most iatrogenic nerve injuries Untidy wounds involve maceration of all tissues in the area: Bony damage could also be current. Surrounding gentle tissue might have been misplaced or rendered nonviable and is expected to heal with vital scarring.
Risperdal 4 mg order
Capsulorrhaphy Dressing Be positive that your assistant maintains the nice toe on the proper position during capsulorrhaphy symptoms 7 weeks pregnant 2 mg risperdal purchase. In our expertise medications rheumatoid arthritis risperdal 3 mg buy generic, at 1 month postoperatively patients could switch to a pair of sentimental and wide lace-up shoes and initiate hallux range-of-motion workouts. In our apply, it takes a median of 3 to four months for patients to attain the utmost range of motion and return to regular shoe wear and full exercise. Recurrence or undercorrection Inappropriate preoperative planning Stretching the indications Usually because of inadequate: Lateral translation Rotation of the first metatarsal head Soft tissue balancing during the capsulorrhaphy Lack of correct postoperative bunion dressing Avascular necrosis of the top of the first metatarsal Overzealous lateral delicate tissue stripping Overpenetration of the saw blade into the lateral capsule Although radiographic first metatarsal head modifications are regularly noticed after distal metatarsal osteotomies, they hardly ever progress to symptomatic necrosis and collapse of the metatarsal head. In these pictures, we can see the correction obtained with the biplanar distal chevron osteotomy. In the lateral view, we are able to see the scale and position of the screw used in the fragment fixation. Lateral views of a patient handled by the biplanar distal chevron osteotomy, the place we are ready to see each the plantar and dorsal arms of the osteotomy, the place of the screw utilized in its fixation, and the alignment of the cephalic fragment with the metatarsal diaphysis ensuing from the dorsal fragment resection. Treatment of hallux valgus with an increased distal metatarsal articular angle: analysis of double and triple first ray osteotomies. We routinely change the bandage for my bunion patients at 10-day intervals to confirm that proper great toe alignment is maintained. Avali��o radiol�gica do h�lux valgo: estudo populacional de novos par�metros angulares. By altering the situation and displacement of the osteotomy, the indications may be expanded to more advanced deformities while preserving the simple surgical exercise. The apex of the chevron osteotomy may be modified to a more proximal location along with a reduced angle to provide a stable healing floor that facilitates maximal lateral translation. The proximal location of the osteotomy also reduces the risk of avascular necrosis and permits safe lateral capsule release wanted for larger corrections. This method facilitates remedy for moderate to extreme bunion deformity with a straightforward surgical method utilizing limited, readily available inside fixation. This line crosses the first metatarsal shaft bisector close to the best location for a corrective osteotomy. The grade of sesamoid subluxation is evaluated to determine whether a lateral capsular launch is indicated. Pertinent to the corrective elements of a translational osteotomy is the width of the distal metatarsal. The amount of correction may be restricted in a small, slender, or "hourglass" formed bone. This further corrective factor should be addressed during the surgical planning. Correction by lateral translation of the distal metatarsal could also be compromised if the cuneiform�metatarsal joint is unstable. The place where this line crosses the first metatarsal bisector helps decide the placement and diploma of translation wanted for the first metatarsal osteotomy. A Freer elevator is useful to probe and establish the dorsal margin of the subluxed lateral sesamoid. Then incise the capsule longitudinally from the phalanx to nicely proximal to the lateral sesamoid. The function of this longitudinal minimize is to allow medialization of the plantar sesamoid complex at the time of capsule restore from the medial facet. Mobilize the tissues to expose the capsule from the medial sesamoid inferiorly to the extensor hallucis longus tendon superiorly. The medial plantar digital nerve is also at risk and must be protected as the dissection nears the medial sesamoid. Reflect the capsule to expose the medial metatarsal eminence and the joint, however pre- serve it on the dorsal or plantar facet to reduce danger of vascular insult. Usually the reduce is 1 to 2 mm medial to the articular margin or the sagittal groove. Next, use a Freer elevator to gently strip the periosteum and soft tissue over the realm where the osteotomy is anticipated to reduce the dorsal and plantar features of the metatarsal. Again, leave the tissues distal to the bone reduce in place to reduce vascular compromise. The osteotomy could be affected by noticed position with a dorsal, plantar, proximal, or distal angulation. After finishing the osteotomy, the distal head fragment ought to be readily mobilized. Translation is facilitated by making use of traction to the toe with one hand and utilizing the other hand to pull with a towel clip on the apex of the proximal metatarsal. Since the osteotomy is often proximal to the metaphyseal bone, the lateral cortex typically appears as a spike. Up to 90% translation is possible and satisfactorily stabilized with Kirschner wires. The osteotomy is translated laterally with traction and thumb stress on the distal end while counterpressure is applied with a towel clip to the medial spike of the proximal end. The lateral cortex of the proximal metatarsal supplies a secure spike to perch the distal head fragment. Pins are sometimes bent and left out percutaneously however may be cut adjoining to the bone and removed electively. Note contact with the medial and lateral facet of the proximal metatarsal earlier than entering the distal head fragment. This must be contoured in line with the medial metatarsal head to avoid signs at this space postoperatively. The quantity of tissue eliminated is judged to allow adequate correction of the hallux valgus. Then carry out a "pants-over-vest" closure between the plantar and dorsal capsule to enhance sesamoid place. A U-shaped wedge of capsule is removed and sutured to tighten the plantar limb of the capsule and correct the hallux valgus. Suture is positioned in a "pants-over-vest" approach to advance the plantar limb of the capsule medial and dorsal. The increased lateral translation of the osteotomy usually decompresses the lateral constructions. An aggressive contouring of the proximal portion of the metatarsal is important to cut back the danger of a residual bony bump close to the osteotomy site. The Kirschner wires have to be positioned proximal enough to avoid being reduce out during this maneuver. Two Kirschner wires are recommended to cut back the risk of head migration until healing callus has developed. They are allowed to "heel walk" in a postoperative shoe with crutches provided for longer distance or ache management. At 5 weeks the pins are removed and the affected person is taught to use a compression wrap and toe spacer. With larger osteotomy translation and correction, radiographic healing can take three months or extra.
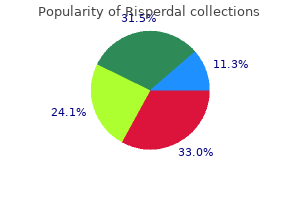
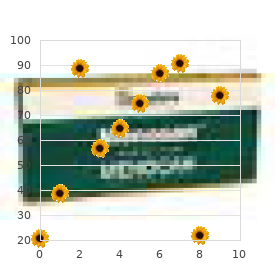
| Comparative prices of Risperdal |
| # | Retailer | Average price |
| 1 | Target | 973 |
| 2 | Dick's Sporting Goods | 824 |
| 3 | Nordstrom | 303 |
| 4 | RadioShack | 452 |
| 5 | Dollar Tree | 716 |
| 6 | Sears Holdings | 943 |
| 7 | Bon-Ton Stores | 140 |
| 8 | Dollar General | 181 |
| 9 | BJ'S Wholesale Club | 209 |
| 10 | OSI Restaurant Partners | 505 |
Risperdal 3 mg mastercard
Another site that has favorable traits when it comes to high quality of graft donor medications xl risperdal 2 mg buy cheap line, as well as therapeutic of donor web site symptoms 9 days past iui generic 2 mg risperdal overnight delivery, contains the scalp. The very wealthy vascular provide to the scalp makes splitthickness pores and skin grafts from this website quite robust. If the harvest is saved within the hair-bearing parts of the scalp, little to no donor defect could be detected as soon as hair has grown back. Moreover, because of the high density of epidermal appendages within the scalp, re-epithelialization of this space is extra rapid than at different sites on the body. This rapid re-epithelialization helps to decrease the potential for donor deformity (ie, scarring and dyspigmentation). Harvest Skin harvest is tremendously facilitated by correct preparation of the chosen site. First, a template of the bed to be grafted ought to be transferred to the donor site to guarantee an enough harvest. Limiting blood loss from the harvest site is desirable and is definitely achieved by pre-injecting the hypodermis of the deliberate harvest space with an epinephrine-containing native anesthetic. If a long-acting native anesthetic similar to Marcaine with epinephrine is used, the affected person could have the extra good thing about prolonged donor website anesthesia postoperatively. As split-thickness donor sites are usually fairly painful, it is a actual profit and is appreciated by the patient. When a big area is deliberate for harvest, consideration should be paid to the suitable maximum dosage for the native anesthetic chosen. Dilute options in these cases can provide the advantages looked for these larger surface areas whereas still respecting the maximum allowed dosages. Microanatomy As advised earlier, the surgeon have to be concerned with the microanatomic situations of the wound mattress. Healthy fats, muscle, paratenon, or periosteum have to be current inside the base of the wound to guarantee success. Additional issues include proper d�bridement of nonviable tissues from the wound mattress in addition to the minimization of bacterial contamination. Donor Sites Glabrous pores and skin the solely real of foot inside the arch, beginning at the junction of glabrous and nonglabrous pores and skin alongside the medial aspect of the arch the ulnar side of the hand, beginning at the junction of the glabrous and the nonglabrous skin alongside the ulnar facet of the palm Full-thickness pores and skin Redundant areas of full-thickness skin out there for harvest that keep ease of major closure of the donor defect include the lower stomach, running from the anterior superior iliac backbone in a delicate arc across the lower portion of the abdomen to the contralateral anterior superior iliac backbone. Depending on necessities of the recipient web site, number of full-thickness skin graft can vary from the relatively hairless portions found laterally to the hirsute areas discovered centrally. Smaller areas of satisfactory full-thickness pores and skin can be harvested from the higher inside arm. This skin, located at the junction of the medial biceps and triceps muscle groups, is skinny and often hairless. Among the most common are traumatic accidents, which commonly result in avulsive lack of pores and skin. Other causes embody burn damage to the upper extremity, as nicely as defects created by tumor elimination. Any certainly one of these mechanisms may end in a broad range of accidents, from simple pores and skin loss to injuries of deeper structures, including loss of paratenon or periosteum. Skin in younger adults is thick and wholesome; nonetheless, in in regards to the fourth decade the pores and skin begins to thin. Despite variations in pores and skin thickness at differing anatomic locations, the general dermal-to-epidermal ratio remains comparatively fixed: about 95% dermis to 5% epidermis. Blood vessels type arborizations into the dermis of the pores and skin via entry portals within the dermal papillae. After utility to an appropriately ready wound bed, both split- and full-thickness grafts bear a course of that has been commonly termed "take. Plasmatic imbibition is the method whereby nutrients and oxygen are drawn into the graft by absorption and capillary motion. This early section of graft support is adopted by inosculation and capillary ingrowth. Once capillary ingrowth occurs and makes contact with the vascular network inherently present throughout the graft, blood flow is re-established, and the skin graft takes on a pinkish hue. The new vascular connections between graft and mattress, in addition to the model new fibrous connections, solidify graft adherence. The phenomenon of main contraction refers to the tendency of a graft to shrink on elevation from the donor website. Substantial main contraction is extra usually related to full-thickness pores and skin grafts than with split-thickness pores and skin grafts. It is clinically essential to remember that the immediate and long-term elasticity of full-thickness skin grafts is far higher that in split grafts. It is this elastic property that makes full-thickness pores and skin grafts an ideal choice for use round joints. Full-thickness grafts tend to stay about the identical size and, for practical functions, show little to no secondary contraction. Full-thickness pores and skin grafts have the capability to enhance their surface space with limb progress over time, whereas split-thickness grafts are probably to lower in dimension by a process of contraction, or, alternatively, their size stays static. Reinnervation the restoration of sensation in skin grafts is mediated via both peripheral ingrowth and direct progress into the graft from the bed. Factors affecting reinnervation of skin grafts embrace the situation and high quality of the recipient mattress, as properly as the choice of full- versus split-thickness pores and skin graft. Timing of recovery is variable, with some sensory restoration at between four and 6 weeks submit grafting. The velocity with which sensory recovery is realized is dependent upon the accessibility of graft neural sheaths to wound mattress nerve fibers. Accessibility of neural sheaths is improved in fullthickness grafts over their split-thickness counterparts, and, therefore, sensory recovery in full-thickness grafts is both more speedy and more complete. Properties of Skin Grafts Skin grafts have been used to present each momentary and everlasting protection, providing the inherent advantage of safety of the host bed from additional trauma whereas also offering an essential barrier to an infection. Split-thickness grafts are inclined to adhere to wound beds extra easily and beneath antagonistic conditions that would not sometimes assist full-thickness graft viability. This attribute of split-thickness skin grafts offers a considerable advantage in managing tough wounds; nevertheless, certain disadvantages can come up from their use. Once healed, split-thickness skin grafts bear secondary contraction which, beneath uncontrolled circumstances, can lead to pathologic contracture. Additional disadvantages arising from the use of splitthickness skin grafts include dyschromia, poor elasticity, and decreased durability when referenced against their fullthickness counterparts. Full-thickness pores and skin grafts embody the full thickness of the dermis, together with the dermis. In the preliminary phases, fullthickness pores and skin grafts have a tendency not to show the hardy "take" often seen with split-thickness pores and skin grafts. To guarantee full-thickness graft success, their use should be restricted to well-vascularized recipient beds only. Once established, full-thickness grafts provide distinct benefits; particularly, secondary contraction is way less problematic.
Risperdal 3 mg order otc
The place of the pinnacle is higher than the tuberosities medication 3 checks risperdal 2 mg buy discount, and adjustments on this relationship will cause impingement symptoms irritable bowel syndrome 2 mg risperdal buy. The humeral head is retroverted roughly 30 degrees (range 20 to 60 degrees). The head is barely higher than the tuberosities, barely medial and posterior to the humeral shaft, retroverted 30 levels. The lateral entry website for locking screw fixation (4�5 cm distal to the tip of the acromion) locations the axillary nerve in danger. Axial load transmitted to the humerus might cause impacted fracture in osteoporotic bone. Violent muscle contractures, as in grand mal seizures and electrical shock, are related to posterior dislocation because of overpowering inner rotators and adductors. Pathologic causes include tumor, multiple myeloma, and metastatic or metabolic issues. Osteoporosis is related to fractures of the proximal humerus (more than any other fracture). In a three-part fracture with intact larger tuberosity, the humeral head is pulled by the supraspinatus and infraspinatus tendons; if the tendons are intact, the humeral head is externally rotated. Rotator cuff tears Neurovascular harm: axillary nerve, brachial plexus Avascular necrosis of the humeral head typically results from disruption of the arcuate artery. The axillary artery additionally may be broken, however less commonly, in fracture-dislocations. In patients youthful than 50 years of age, violent trauma, contact sports, and falls from heights are answerable for fractures. Acute, recurrent, or chronic dislocation without major Indications Two-part proximal humerus fracture Three-part proximal humerus fracture Certain four-part proximal humerus fractures Prerequisites Shoulder table, image intensification, and experienced radiology technician Be conscious of the learning curve (do not attempt nailing of a four-part fracture before buying enough experience with two- and three-part fractures). The muscular attachments of the larger and lesser tuberosities will cause abduction, external rotation, and inner rotation, respectively. A bolster is used to elevate the shoulder from the desk and to allow shoulder extension. Extension of the shoulder is critical to expose the entry site within the humeral head. Flexion of the shoulder will result within the acromion overlying the middle of the humeral head within the sagittal plane, obscuring the entry site or errantly directing an entry angle. Anterior cutout of the nail within the head fragment can easily happen in an osteoporotic humeral head with an associated higher tuberosity fracture. Contraindication: head-splitting, comminuted displaced humeral head fragment devoid of soft tissue attachment Preoperative Planning Successful intramedullary nailing of the proximal humerus fracture is determined by consistent integration between picture intensification and the surgical steps. Patient positioning on a radiolucent desk will enable the surgeon to use a minimally invasive strategy. Any error on the entry site will trigger inevitable problems with the rest of the procedure. Positioning Positioning on the desk must permit orthogonal and overhead axillary views. Intramedullary nailing for isolated surgical neck fractures could additionally be performed fully percutaneously using a lot of the methods described in the following paragraphs. However, when tuberosity reduction and fixation are required, a wider approach usually is critical. The timing of the open method is decided by the sequencing of head, shaft, and tuberosity fixation. In the technique we describe in this chapter, head�shaft fixation is accomplished percutaneously utilizing nailing and interlocking screws earlier than tuberosity fixation. Alternatively, an open approach with tuberosity reduction and fixation could be performed before nail insertion. The wires should be separated by sufficient distance to allow insertion of the nail between them (1. The K-wires must be directed within the longest axis of the humeral head within the axial plane. Confirmation of the right placement within the axial airplane is done by the overhead axillary view. Then the C-arm is positioned to view the development of the pins within the coronal plane projection. Unfortunately, with inner rotation, extension also occurs in the humerus and the humeral head, depending on the soft tissue attachments. This initial pin will serve to orient the humeral head, specifically the specified diploma of retroversion. Image intensification can be utilized to place a K-wire via the top according to intramedullary axis of the humerus. To achieve fracture reduction, the joysticks within the proximal fragment should be used to rotate the top whereas concurrently rotating the distal shaft manually to obtain true orthogonal views of the top in reference to the shaft. Combining rotation of the pinnacle fragment (K-wires) with the shaft (arm) is used to assist in fracture reduction. Manipulation of the fracture fragments with the K-wires allows disimpaction of the fracture, bettering the varus or valgus alignment. The anterior edge may be troublesome to palpate and to differentiate from the humeral head because of edema and hematoma from the fracture. Manipulation of the proximal fragment has been the one reliable approach to establish appropriate placement. The reamer is inserted over the guidewire, and the gentle tissues are retracted and guarded. The reamer is advanced through the rotator cuff in "reverse" till bone contact, then on "ahead" via the humeral head. The guidewire that was used to initiate the entry web site is removed, and a longer guidewire is passed to the shaft fragment. On some occasions, even exterior fixator placement from the scapular spine to the distal humerus is necessary. The external fixator is applied and distraction accomplished with manipulation of the proximal aspect of the shaft; guidewire passage normally is easy. Usually, impaction of the distal fragment by blows in opposition to the olecranon, while supporting the proximal humeral head indirectly by way of the gentle tissues, is adequate. The objective of this screw is to connect the top to the shaft earlier than fixation of the tuberosities. Careful blunt dissection to bone, drilling throughout the sheath, and inserting the screw inside the confines of the sheath are essential. It is sometimes useful to take away the drill after which use a blunt guidewire and guarantee good humeral head subchondral bone contact earlier than further drilling or screw placement. This step should circulate very smoothly if the initial K-wires have been positioned in the right axial aircraft alignment. Errant placement or acceptance of poorly positioned K-wires will outcome only in further deviation. However, sufferers with osteoporosis do have a threat of the fracture fragment settling.
Generic 2 mg risperdal with amex
The deltopectoral interval is developed by retracting the pectoralis main medially and the deltoid laterally treatment ulcerative colitis purchase risperdal 2 mg otc. The lateral border of the conjoint tendon is recognized and the brief head of the biceps (supplied by the musculocutaneous nerve) and coracobrachialis (supplied by the musculocutaneous nerve) are displaced medially to enable entry to the anterior aspect of the shoulder joint treatment skin cancer risperdal 3 mg order on line. Simple medial retraction of the conjoined tendon may be sufficient for a process similar to subscapularis repair or capsular restore. If more exposure is critical, the conjoint tendon could be detached with the tip of the coracoid course of. The axillary artery is surrounded by cords of brachial plexus, which lie behind the pectoralis minor muscle. To decrease danger for nerve harm, the arm must be stored adducted whereas work is being accomplished across the coracoid process. Remember, the musculocutaneous nerve enters the coracobrachialis on its medial facet. Overly aggressive retraction could cause a neurapraxia of the musculocutaneous nerve. Behind the conjoined tendon of the coracobrachialis and the quick head of biceps lies the subscapularis muscle. Externally rotating the arm brings the subscapularis further into the operative subject. This maneuver will increase the space between the subscapularis and axillary nerve because it disappears below the decrease border of the muscle. Identifiable landmarks on the inferior border of the subscapularis are three small vessels (from the anterior humeral circumflex artery) that run transversely and often require ligation or cauterization. These vessels run as a triad (often known as the "three sisters"): a small artery with its two surrounding venae comitantes. There are numerous methods of taking down the subscapularis as per surgeon choice. Some divide the subscapularis 1 to 2 cm from its insertion onto the lesser tuberosity. Inferior border of the subscapularis is the easiest location to enable separation between the subscapularis and capsule. The capsule is incised longitudinally to enter the joint wherever the chosen repair must be performed. Axillary incision starting inferior to the tip of the coracoid and progressing toward the anterior axillary fold. In this dissection, the subscapularis tendon is being tagged on the superior border of the rotator interval. Subperiosteally, the anterior deltoid is elevated from the acromion and the acromioclavicular joint. Continue the detachment by sharp dissection laterally to expose the anterior side of the acromion. Bleeding will be encountered throughout this dissection as a outcome of the division of the acromial branch of the coracoacromial artery. Stay sutures are inserted in the apex of the split to prevent the muscle from inadvertently splitting distally during retraction and damaging the axillary nerve. A transverse incision begins on the anterolateral corner of the acromion and ends just lateral to the coracoid. The posterior curve of the deltoid incision may be moved more posteriorly, as depicted right here, to enable needed publicity as dictated by the pathology. The break up edges of the deltoid muscle are retracted to reveal the underlying coracoacromial ligament. The supraspinatus tendon with its overlying subacromial bursa now may be visualized. The head of the humerus is rotated to expose completely different parts of the rotator cuff. Horizontal incision along the scapular spine allowing for the posterior method to the shoulder. Cadaveric specimen depicting the internervous airplane between the infraspinatus and teres minor as well as the axillary nerve within the quadrangular area. Incision A longitudinal incision is remodeled the tip of the coracoid process of the scapula; it runs distally and laterally in the line of the deltopectoral interval to the insertion of the deltoid muscle on the lateral aspect of the humerus, about halfway down its shaft. Surgical Dissection the origin of the deltoid is identified on the scapular spine. There are 3 ways to manage the deltoid throughout posterior exposures: Detach the origin on the scapular backbone Split the deltoid muscle alongside the size of its fibers Elevate the deltoid from the inferior margin the plane between the deltoid muscle and the underlying infraspinatus muscle is identified. The axillary nerve runs longitudinally within the quadrangular space beneath the teres minor. The posterior circumflex humeral artery runs with the axillary nerve in the quadrangular house between the inferior borders of the teres minor muscle. Surgical Dissection Proximal Humeral Shaft the deltopectoral interval is recognized using the cephalic vein as a guide and the two muscle tissue are separated, retracting the cephalic vein both medially with the pectoralis main or laterally with the deltoid. The internervous airplane between the deltoid muscle and the pectoralis main muscle. Further distally, one can appreciate the internervous aircraft between the medial fibers of the brachialis (musculocutaneous nerve) medially and the lateral fibers of the brachialis (radial nerve) laterally. Deltopectoral incision: developing the interval between the deltoid and pectoralis main. With deeper dissection, the biceps tendon is seen running within the rotator interval. Further distal dissection reveals the musculocutaneous nerve passing alongside the medial border of the biceps muscle. To expose the distal third of the humerus, the fibers of the brachialis are split. Flexion of the elbow will relieve the strain off the brachialis, making the publicity simpler. To expose the bone fully, the surgeon might must detach part or all the insertion of pectoralis major muscle. The minimum amount of sentimental tissue ought to be detached to allow enough visualization and reduction of the fracture. If further publicity is required, the surgeon dissects medially in a subperiosteal manner to keep away from injury to the radial nerve, which lies within the spiral groove of the humerus and crosses the back of the middle third of the bone in a medial to lateral course. Distal Humeral Shaft the surgeon identifies the muscular interval between the biceps brachii and brachialis. The fibers of the brachialis are split longitudinally within the interval between the medial 2/3 and the lateral 1/3 to expose the periosteum on the anterior surface of the humeral shaft. In the anterior compartment of the distal third of the arm, the radial nerve pierces the lateral intermuscular septum and lies between the brachioradialis and brachialis muscular tissues. The medial head, which is the deepest, has a twin nerve supply (radial and ulnar nerves).
Risperdal 3 mg on line
Clinical manifestations of vasospastic problems vary from episodic digital vasospasm and ache medicine logo buy cheap risperdal 4 mg, to extreme hand and digit ischemia symptoms after hysterectomy risperdal 4 mg line, progressing to gangrene. Vaso-occlusive problems observe a more predictable medical course in that they normally end result from mounted lesions that are progressive. Cold intolerance and vasomotor colour adjustments within the hand develop, forcing patients to search therapy. Does the affected person describe paresthesias, pallor, cold intolerance, pain, digit ulceration The complete upper extremity is examined for range of movement, pores and skin colour and turgor, capillary refill, radial and ulnar pulses, temperature, and presence of ulcerations. The radial and ulnar pulses are palpated and examined by Doppler probe if needed. The palmar arch is assessed with the Doppler probe in addition to the radial and ulnar digital arteries to every finger. The arterial flow is then re-established to the hand sequentially by releasing the radial and ulnar arteries, and capillary refill is assessed. This check evaluates the patency of arterial inflow to the hand by way of the radial and ulnar arteries. Buerger disease (thromboangiitis obliterans): an inflammatory occlusive illness of the small and medium-sized vessels of the limbs Arteritis: a group of problems characterized by acute or persistent inflammation within the walls of small, medium, and large arteries. Patients with these conditions usually current with concurrent fever, malaise, weight loss, cutaneous lesions, and arthralgias. Avoidance of smoking and publicity to chilly temperatures may control vasospastic episodes. Biofeedback Patients are skilled to management sure bodily processes that occur involuntarily. Electrodes are attached to the pores and skin of the patient and physiologic responses monitored. The biofeedback therapist then leads the affected person by way of exercises that result in desired physical modifications. Occlusive dressings could also be useful both to protect areas from recurrent trauma and to promote healing of lesions. Calcium channel blockers, eg, nifedipine Pentoxifylline decreases blood viscosity and should result in enjoyable vascular smooth muscle. Indications for a digital sympathectomy are progressive signs of Raynaud syndrome or ulcerations refractory to medical management with no proof of major occlusion of the radial or ulnar arteries and with good visualization of three frequent digital arteries in the palm. Cold challenges are very painful for patients with scleroderma and systemic lupus erythematosus and are used on a case-by-case basis. The patient should be educated on the outcomes of the varied procedures and realize the limitations of every one. Positioning the affected person is placed within the supine place on the operating room table with the extremity on an appropriately padded hand desk. If a vein graft is anticipated, one other extremity (usually a leg) is prepped and a proximal tourniquet utilized. Approach Usually, the hand surgeon should access proximal arterial inflow vessels when treating either vasospastic or vasoocclusive problems of the hand. The brachial artery in the higher arm is approached by way of an incision on the medial side of the arm. The distal brachial artery and proximal radial and ulnar arteries are approached by way of a lazy S incision within the antecubital fossa. Care is taken to keep away from making a straight line incision across the antecubital fossa. The radial and ulnar arteries within the forearm are approached through a longitudinal incision over the precise vessel. The palmar arches are accessed via Bruner incisions extending proximally from the proximal phalanges, using natural creases in the palm where attainable, or through an inverted J-shaped incision within the palm. The digital arteries are approached through Bruner incisions on the palmar side of the finger or through a midlateral incision on the digit. Proximal or cervical sympathectomy has largely fallen out of favor because of the excessive recurrence rates. Peripheral sympathectomy has gained popularity since Pick17 recognized sympathetic nerve fibers innervating the arteries from the wrist to the fingers. This should be performed very fastidiously to keep away from damaging the digital arteries themselves. View through the operating microscope earlier than (A) and after (B) removing of the adventitia from a typical digital artery. Radical or intensive digital sympathectomy earlier than (C) and after (D) stripping the adventitia from the distal ulnar artery, superficial palmar arch, and customary digital arteries to the index�middle, middle�ring, and ring�small finger net areas. It also sometimes is used to treat a thrombosed or occluded ulnar artery in hypothenar hammer syndrome. Adequate arterial inflow and patent distal arteries with enough distal "run-off" are present. Reverse vein grafts (eg, cephalic, saphenous) or arterial grafts (eg, deep inferior epigastric artery, lateral circumflex artery, thoracodorsal artery) are harvested in the usual fashion. An end-to-side anastomosis of the graft to the influx artery is preferable to maximize any remaining circulation to the hand, but end-to-end anastomoses are technically easier. The distal anastomosis often is end-to-end to the superficial or deep palmar arches or end-to-side to the common digital arteries. After the anastomoses have been completed, the tourniquet is deflated, and vascular influx by way of the opposite artery is occluded by manual compression for a couple of minutes to maximize circulate across the anastomoses. Restoration of arterial circulate into the hand is assessed both by using a pencil Doppler probe or by performing an Acland "adventitial strip test" distal to the distal anastomosis. Microsurgical revascularization for thrombosis or occlusive disease of the distal ulnar artery and superficial palmar arch, utilizing an interposition vein graft from the ulnar artery to the frequent digital arteries. Microvascular revascularization for thrombosis or occlusive illness of the distal radial artery and deep palmar arch, using an interposition vein graft from the radial artery to the princeps pollicis artery. Small Fogarty embolectomy catheters could additionally be used selectively at the arm, elbow, forearm, and wrist levels, but use of embolectomy catheters within the hand and digits is difficult and may itself result in vascular damage. Insert the Fogarty catheter into the artery, and cross it down the lumen past the area of occlusion; then inflate the balloon. This is repeated till the lumen is totally cleared of the embolus, as demonstrated by improved backbleeding from the distal vessel. Assess the restoration of arterial move into the hand both by utilizing a pencil Doppler probe on the artery more distally or by performing an Acland "adventitial strip check" distal to the positioning of embolism. Ligate the vein proximally and perform an end-to-side microsurgical anastomosis between the vein and the radial or ulnar artery on the wrist. After the anastomosis has been performed, assess arterial flow via the distal vein. Any remaining obstruction due to a valve must be relieved by an open valvulotomy and excision of the valve leaflets, followed by microsurgical closure of the vein. Postoperative monitoring is carried out utilizing a pencil Doppler probe over the distal arterialized vein to the fingers. A discrete segment of thrombosed or occluded artery have to be identified for this to be efficient. Identification of an embolus must be handled with heparinization instantly to stop propagation of the clot.
Generic risperdal 3 mg otc
When full vary of movement has been obtained symptoms carpal tunnel discount 2 mg risperdal overnight delivery, mild progressive strengthening and resumption of normal activities start medicine 2000 2 mg risperdal cheap amex. Most have been case stories, a collection of three or four patients, or a discussion of the complications of the harm or its treatment. Sadr and Swann24 and Rockwood and Odor22 have both documented the nice long-term results obtained with nonoperative remedy of atraumatic sternoclavicular instability. De Jong7 has documented good long-term leads to 13 patients with anterior dislocations treated nonoperatively. Several bigger series9,eleven,29 have reported on a few dozen patients handled with open discount, ligament repair or reconstruction, and fixation with pins or sternoclavicular wiring. Eskola,10 nevertheless, noted a excessive failure price if the remaining medial clavicle was not efficiently stabilized to the primary rib. In a separate study, Rockwood et al21 reported on seven patients who had beforehand undergone medial clavicle resection with out ligament reconstruction. Worman and Leagus30 reported that 16 of 60 sufferers with posterior dislocations had suffered complications of the trachea, esophagus, or nice vessels. Errors of patient choice Operating in unindicated circumstances introduces another set of problems. Twenty-nine managed with out surgery had no limitations of exercise or life-style at over eight years common follow-up. Eight handled (elsewhere) with surgical reconstruction had elevated ache, limitation of exercise, alteration of life-style, persistent instability, and significant scars. Before surgery, most of these sufferers had minimal discomfort and wonderful motion and complained only of a "bump" that slipped in and misplaced with certain motions. Intraoperative issues Little has been written about these, but a veritable jungle of vitally important structures lurks immediately behind the sternoclavicular joint. We at all times perform these operations with an available, in-house cardiothoracic surgeon on notice and request his or her presence in the working suite for all but the most routine instances. Postoperative complications Hardware migration: Because of the movement on the sternoclavicular joint, super leverage is utilized to pins that cross it; fatigue breakage of the pins is widespread. Numerous authors have reported deaths and many near-deaths from Kwires and Steinmann pins migrating into the heart, pulmonary artery, innominate artery, aorta, and elsewhere within the mediastinum. Despite numerous admonitions in the literature regarding the usage of sternoclavicular pins, there have been continued reviews of intrathoracic K-wire migration, most recently in 2005. As noted above, each Rockwood21 and Eskola10 noted vastly inferior outcomes when the residual medial clavicle was not stabilized to the first rib, and an incapability to get hold of equal results when the costoclavicular ligament was reconstructed in a delayed style. This leaves the extremity without a "strut" connecting it to the thorax but can produce substantial relief of pain and improvement in motion and activity. Direct observations on the perform of the capsule of the sternoclavicular joint within the clavicular assist. Interposition arthroplasty with bone-tendon allograft: a technique for therapy of the unstable sternoclavicular joint. Balser plate stabilization: an alternate therapy for traumatic sternoclavicular instability. Treatment of posterior epiphyseal disruption of the medial clavicle with a modified Balser plate. Epiphyseal fracture�retrosternal dislocation of the medial finish of the clavicle: a case report. Posterior sternoclavicular dislocation in a rugby participant as a explanation for silent vascular compromise: a case report. Using the semitendinosus tendon to stabilize sternoclavicular joints in a patient with Ehlers-Danlos syndrome: a case report. Ligamentous restraints to anterior and posterior translation of the sternoclavicular joint. Short-term outcomes after surgical therapy of traumatic posterior sternoclavicular fracturedislocations in kids and adolescents. Conservative administration of a displaced medial clavicular physeal harm in an adolescent athlete. Chapter 13 Medial Clavicle Excision and Sternoclavicular Joint Reconstruction John E. Other conditions embrace rheumatoid arthritis, seronegative spondyloarthropathies, crystal deposition disease, sternoclavicular hyperostosis, condensing osteitis, and avascular necrosis. When suspected, the sternoclavicular joint ought to be aspirated for culture, Gram stain, and cell counts after which handled with irrigation and d�bridement. Traumatic instability is outlined by the path of displacement of the clavicular head and is superior, anterior, or posterior. Posterior instability has been related to a big selection of doubtlessly fatal comorbidities. Atraumatic instability is usually anterior and is usually seen in people with generalized ligamentous laxity. Symptomatic traumatic instability is greatest treated with closed discount and potential reconstruction of the joint, not resection of the clavicle head. The clavicle pivots over the first rib, dislocating the head of the clavicle posteriorly. Direct blows to the sternoclavicular joint can also dislocate the clavicle head posteriorly. This is particularly true with the pain and swelling seen in perimenopausal women. Infection could present with a relatively benign scientific picture however will progress and should turn out to be severe. It is uncommon for the sternoclavicular joint to be the first joint concerned in rheumatologic situations or crystal deposition illness. Important ligamentous restraints to motion embrace the anterior capsule (restrains anterior and posterior translation), the posterior capsule (restrains posterior translation),10 and the costoclavicular ligament (which is the pivot point for movement in the axial plane). Osteoarthritis is most commonly seen in male laborers, in women in the perimenopausal years, and after radical neck dissection. Rheumatologic disorders can have an result on the sternoclavicular joint as a half of the systemic disease. Other atraumatic conditions are much less frequent and the pathogenesis is essentially unknown. The clavicle pivots over the first rib, forcing the pinnacle of the clavicle anteriorly. Traumatic instability might outcome from high-energy injuries (eg, motor vehicle collision) or may be related to contact in athletics. Posterior instability may be life-threatening because the clavicular head might compress vascular constructions, the trachea, or the esophagus. Atraumatic instability might have an insidious onset and is commonly associated with other indicators of generalized ligamentous laxity (eg, patellar subluxation, glenohumeral subluxation). Arteriography must be thought of in posterior dislocations if vascular harm is suspected. Osteoarthritis, rheumatoid arthritis, seronegative spondyloarthropathies, and sternoclavicular hyperostosis are sometimes bilateral, with gentle ache, and rare erythema.